European Journal of Neurodegenerative Diseases 2017; 6(2) July-December: 17-19
ASTROCYTES PLAY A CRUCIAL ROLE IN TRAUMATIC BRAIN INJURY
Letter to the Editor
S. Saggini 1* and M. Rosati 2
1 Physical and Rehabilitation Medicine, Department of Medical Oral and Biotechnological Sciences, “Gabriele D’Annunzio” University, Chieti-Pescara, Italy;
2 Pescara Civil Hospital, Pescara, Italy.
*Correspondence to:
Professor Raoul Saggini,
Department of Neuroscience and Imaging,
University G. D’Annunzio of Chieti-Pescara,
Chieti, Italy.
e-mail: raoul.saggini@unich.it
KEYWORDS: astrocyte, CNS, brain trauma, pathophysiology, neurodegeneration, inflammation
INTRODUCTION
A traumatic brain injury (TBI) consists of physical damage to the brain tissue and is a major global cause of morbidity and disability, carrying a high socioeconomic burden (1). The damage from a TBI can be either temporary or permanent and compromises the normal functioning of the brain. There can be different types of brain injuries and the course and therapy depend on the location and severity of the damage. The pathological process that occurs after TBI is complex and many factors are involved. In recent years, this topic has been strongly debated in the scientific literature, and the in-depth study of new technologies and various therapies have led to a notable improvement in managing patients with TBI.
Astrocytes, which take their name for their star-like appearance, are important cells of the central nervous system (CNS) and spinal cord. Astrocytes constitute neuroglia and are found in both white matter and gray matter where they present some differences. They participate in many brain functions such as immune reactions, brain diseases, and trauma, with different and sometimes opposing responses. Astrocytes and macrophages are activated early by brain damage, resulting in the release of neurotoxic factors and the subsequent formation of scar tissue (2). After brain trauma, endogenous neurogenesis can occur, which contributes to spontaneous hospitalization after the damage. In this article, we discuss the functions of astrocytes within the CNS and their pathophysiological functions in TBI, which are important topics for developing new therapies.
DISCUSSION
TBIs can be separated into two types of injuries: “primary” injuries, which refers to the mechanical damage that is inflicted, and “secondary” injuries, which refers to the molecular and biological processes that occur after the initial damage. In the “primary” lesion, there is large-scale brain damage that triggers the “secondary” lesion, which consists of extensive inflammation in the CNS. This inflammatory reaction is a defensive response to the physical trauma but can also significantly aggravate the traumatic brain damage. In the “primary” lesion, immune cells including microglia, are activated. The activation of immune cells can improve the traumatic state since they synthesize helpful molecules such as growth factors. However, activated immune cells can also produce inflammatory cytokines and can therefore be very harmful to the ongoing pathological process. For this, developing new immunological strategies could be of great help in tackling this serious problem which too often leads to patient death (3).
Sterile inflammation is a process that always occurs in trauma, and results during the “secondary” injury in TBI (4). This is inflammation that occurs without a response to pathogens, and in which multiple types of cells participate. When an injury takes place, immune cells are recalled and activated by the immune system. These cells then go on to send signals to neurons and glia, causing them to produce inflammatory molecules such as chemokines and cytokines.
Microglial cells are elements of the non-specific innate immune response that promptly respond to antigens that are foreign to the organism, although they sometimes also react against self-antigens (autoimmunity). Microglia express toll-like receptors (TLRs) to recognize pathogens and dangerous molecules, and activation of these receptors leads to the synthesis of inflammatory proteins such as chemokines and cytokines (5).
The first lesion causes a rapid primary response, warning that the brain has suffered trauma with the release of molecules such as ATP and high mobility group box 1 (HGMB1) protein, effectors of the inflammatory state (6,7). These signals lead to the activation of TLRs, which activate myeloid cells including microglia. Furthermore, the assembly of the inflammasome (NALP1) leads to the synthesis of IL-1 and IL-18, two highly inflammatory cytokines, as well as chemokines (8) (Fig. 1). This entire reaction leads to the participation of other molecules, such as reactive oxygen species (ROS) and nitric oxide (NO), which further amplify the inflammatory response.
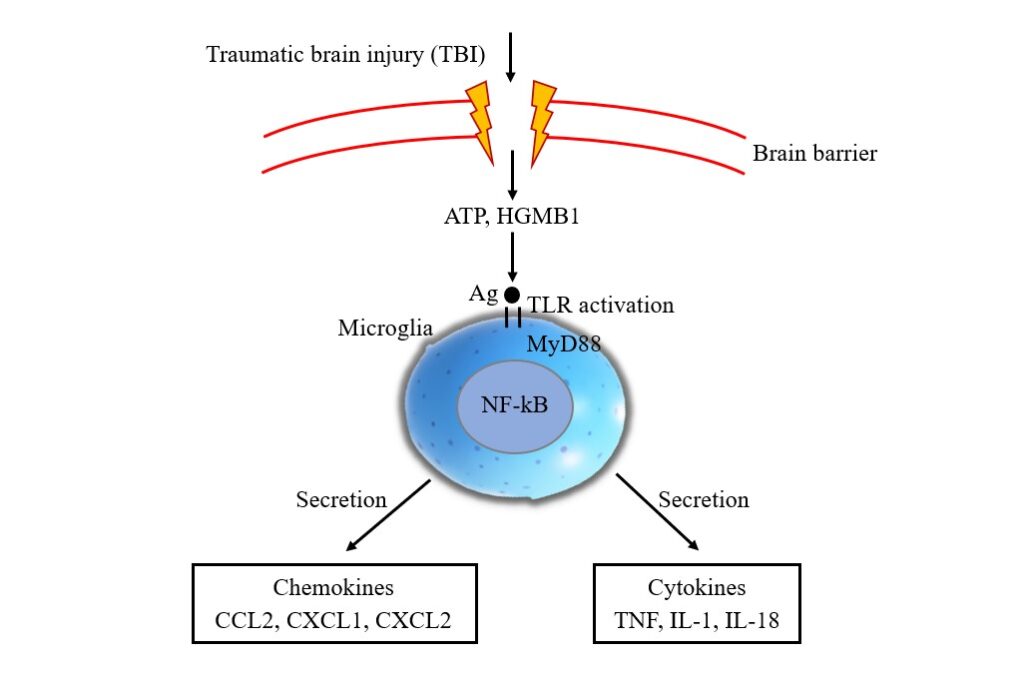
Fig. 1. Traumatic brain injury (TBI) activates ATP, HGMB1, and antigen binding toll-like receptor on microglia cells. This reaction leads to the activation of a cascade involving MyD88 in the cytoplasm and NF-kB in the nucleus, with secretion of CCL2, CXCL1, and CXCL2 chemokines and TNF, IL-1, and IL-18 cytokines.
The innate immune response is followed by a more specific adaptive response, with the activation of T and B lymphocytes that recognize the antigen presented by the antigen presenting cells (APC). The CD4 and CD8 T cell subclasses may have TBI-aggravating cytotoxic functions or may be helpful and regulatory. However, these cells also produce pro-inflammatory cytokines, such as TNF and IL-1, which exacerbate neuroinflammation (9). B cells participate in the activation of T lymphocytes by producing immunoglobulins. Among the latest cytokines discovered are IL-37 and IL-38 that are reported to be anti-inflammatory (10). Since pro-inflammatory cytokines exacerbate the pathological state of TBI, there is a potential role for these cytokines to be used in TBI therapy.
CONCLUSIONS
Following TBI, the activation of immune cells is helpful to repair damage, but on the other hand, the release of inflammatory cytokines and chemokines can be detrimental with neuroinflammation and aggravation to the damaged tissue. Modulation of the immune system that induces sterile inflammation could change the clinical-pathological course following TBI and therefore, more research should continue to resolve the ongoing questions.
Conflict of interest
The authors declare that they have no conflict of interest.
REFERENCES
- World Health Organization. World report on disability. www.who.int. Published 2011. http://www.who.int/disabilities/world_report/2011/en/
- Karve IP, Taylor JM, Crack PJ. The contribution of astrocytes and microglia to traumatic brain injury. British Journal of Pharmacology. 2015;173(4):692-702. doi:https://doi.org/10.1111/bph.13125
- Menon DK. Unique challenges in clinical trials in traumatic brain injury. Critical Care Medicine. 2009;37(Supplement):S129-S135. doi:https://doi.org/10.1097/ccm.0b013e3181921225
- Cederberg D, Siesjö P. What has inflammation to do with traumatic brain injury? Child’s Nervous System. 2009;26(2):221-226. doi:https://doi.org/10.1007/s00381-009-1029-x
- Goodall KJ, Poon IKH, Phipps S, Hulett MD. Soluble Heparan Sulfate Fragments Generated by Heparanase Trigger the Release of Pro-Inflammatory Cytokines through TLR-4. Srinivasula SM, ed. PLoS ONE. 2014;9(10):e109596. doi:https://doi.org/10.1371/journal.pone.0109596
- Laird MD, Shields JS, Sukumari-Ramesh S, et al. High mobility group box protein-1 promotes cerebral edema after traumatic brain injury via activation of toll-like receptor 4. Glia. 2013;62(1):26-38. doi:https://doi.org/10.1002/glia.22581
- Balu R. Inflammation and Immune System Activation After Traumatic Brain Injury. Current Neurology and Neuroscience Reports. 2014;14(10). doi:https://doi.org/10.1007/s11910-014-0484-2
- de Rivero Vaccari JP, Dietrich WD, Keane RW. Activation and Regulation of Cellular Inflammasomes: Gaps in Our Knowledge for Central Nervous System Injury. Journal of Cerebral Blood Flow & Metabolism. 2014;34(3):369-375. doi:https://doi.org/10.1038/jcbfm.2013.227
- González H, Pacheco R. T-cell-mediated regulation of neuroinflammation involved in neurodegenerative diseases. Journal of Neuroinflammation. 2014;11(1). doi:https://doi.org/10.1186/s12974-014-0201-8
- Dinarello CA, Arend WP, Sims JE, et al. IL-1 family nomenclature. Nature immunology. 2010;11(11):973-973. doi:https://doi.org/10.1038/ni1110-973

